People aged between 60 and 74 are being urged to complete a home testing kit that can detect signs of bowel cancer, as part of Humber and North Yorkshire Cancer Alliance’s #flushawaybowelcancer campaign.
April is Bowel Cancer Awareness Month and the Cancer Alliance is carrying out a wide range of activities to raise awareness of bowel cancer symptoms and encourage more people to complete the Faecal Immunochemical Test (FIT) throughout the month.
Activities include:
- Parkruns – members of the Cancer Alliance and partners wearing fancy dress, including fake bums, in York, Beverley, Hull and Cleethorpes
- Cancer Champions – Bite-sized online bowel cancer awareness sessions
- Community events – Awareness activity sessions at leisure centres, supermarkets and other community spaces
- Teaming up with partners – Including Bowel Cancer UK’s Bowel Cancer Awareness Roadshow, visiting Hull 16-18 April, and events with Care Plus Group throughout Grimsby
Click here for information on all the activity near you.
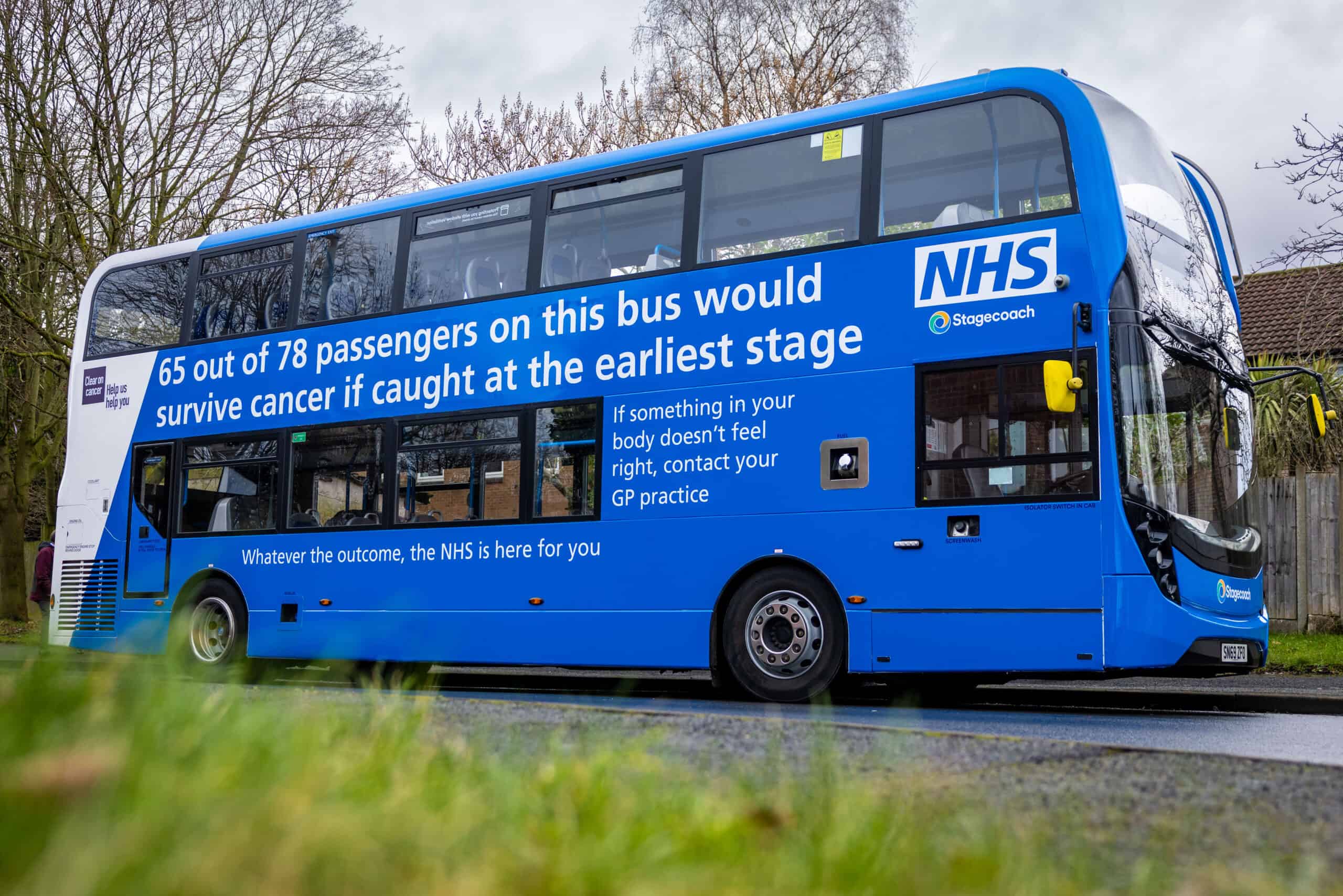
Bowel cancer is the fourth most common cancer in the UK, killing more than 16,800 people every year. However, this type of cancer is curable, especially if diagnosed early, when you are up to nine times more likely to be successfully treated. Nearly everyone survives bowel cancer if diagnosed at the earliest stage. However, this drops significantly as the disease develops.

Andy, 68, raising awareness of the importance of early detection, after his FIT result detected abnormalities.
Screening is one of the best ways to detect bowel cancer early, and Andy Thompson, 68, from Anlaby, East Yorkshire, is keen to raise awareness of the importance of early detection, after his FIT result detected abnormalities which could have developed into cancer.
He said: “To anyone who receives a FIT in the post and is feeling squeamish, I would tell them about my experience compared with a relative of mine. The test isn’t as gruesome as some might think. It only takes a couple of minutes to complete. It probably takes longer to write out your details and return in the post.
“My result came back abnormal, so I had to have further investigations. Fortunately, all they found were polyps, which can become cancerous, so I had them all removed.
“We’re really lucky to get the FIT screening kit for free in the post. For a few minutes of unpleasantness, it can help you detect bowel cancer, or, in my case, help stop you getting it in the first place. Don’t flush away that chance, flush away bowel cancer instead!”
About five years previous, a close relative of Andy’s received a FIT in the post, put it away and forgot about it. A few months later, he was in a lot of pain, and showing symptoms of bowel cancer. Six to eight months after not doing the FIT, he was diagnosed with stage three bowel cancer.
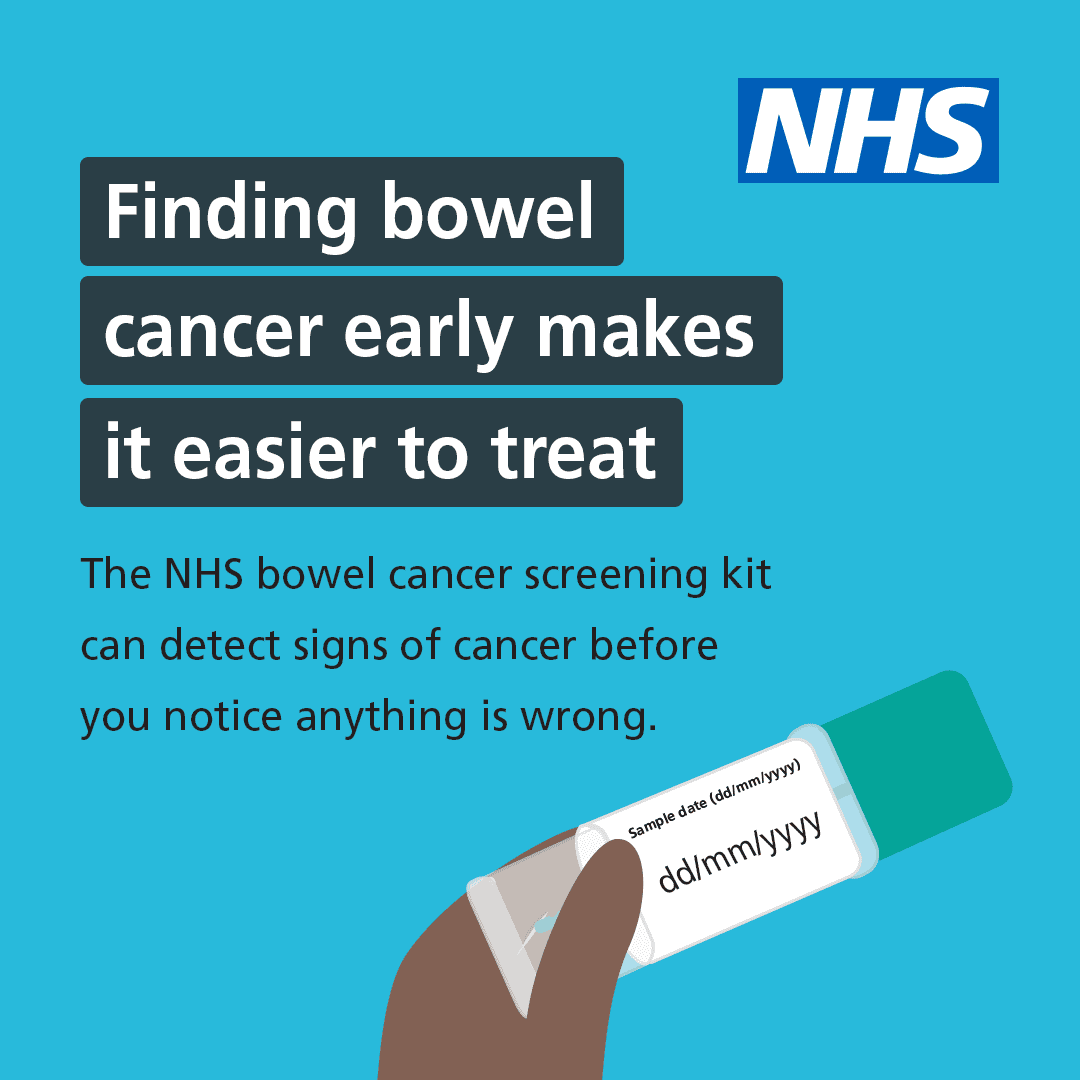
If you are sent a FIT kit, you can complete the test in your own bathroom, next time you poo. Simply follow the step-by-step instructions to:
- collect one tiny sample of poo, using the plastic stick
- pop it in the sample bottle
- post it for free to be tested
The test works by checking for tiny traces of blood – not always visible to the naked eye. If something is found, you will be invited for further tests, usually at a hospital.
Dr Dan Cottingham, Cancer Research UK GP Lead for Humber and North Yorkshire Cancer Alliance, said: “Nine out of 10 new cases of bowel cancer are diagnosed in people over the age of 50, and the earlier it’s treated, the more likely you are to be treated successfully. That’s why it’s so important you don’t ignore the FIT kit when it arrives in the post.
“Don’t flush away that chance of early detection – it’s the most important job you can do for your loved ones.”
Early detection increases your chance of surviving bowel cancer, so knowing what symptoms to look out for is important.
Contact your GP if you have any of these bowel cancer symptoms:
- changes in your poo, such as having softer poo, diarrhoea or constipation
- needing to poo more or less often than usual
- red or black blood in your poo
- bleeding from your bottom
- often feeling like you need to poo, even if you’ve just had one
- tummy pain
- a lump in your tummy
- bloating
- losing weight without trying
- feeling very tired
Bowel cancer awareness will be spread across the Cancer Alliance’s social media channels too, using the hashtag #flushawaybowelcancer. Follow the Cancer Alliance on Facebook and X (formerly Twitter) to help share their messages.
If you or a loved one needs information on, or support for bowel cancer, visit the Cancer Alliance website to be signposted to local bowel cancer support groups.
Visit the Cancer Alliance’s Bowel Cancer Awareness Month webpage to find out more.